The Hair Pull Test: A Non-invasive Tool for Hair Loss Monitoring
For a healthy adult, losing around 80 to 100 hairs in the telogen stage per day is normal.
However, if someone experiences a significant increase in hair loss or notices anagen hair loss
(hair falling out before reaching its full length), it could indicate underlying health issues.
Doctors often rely on quick and non-invasive clinical examinations, such as the hair pull test, to address these concerns.
This article explores the hair pull test, its significance, and its limitations.
Understanding the hair pull test
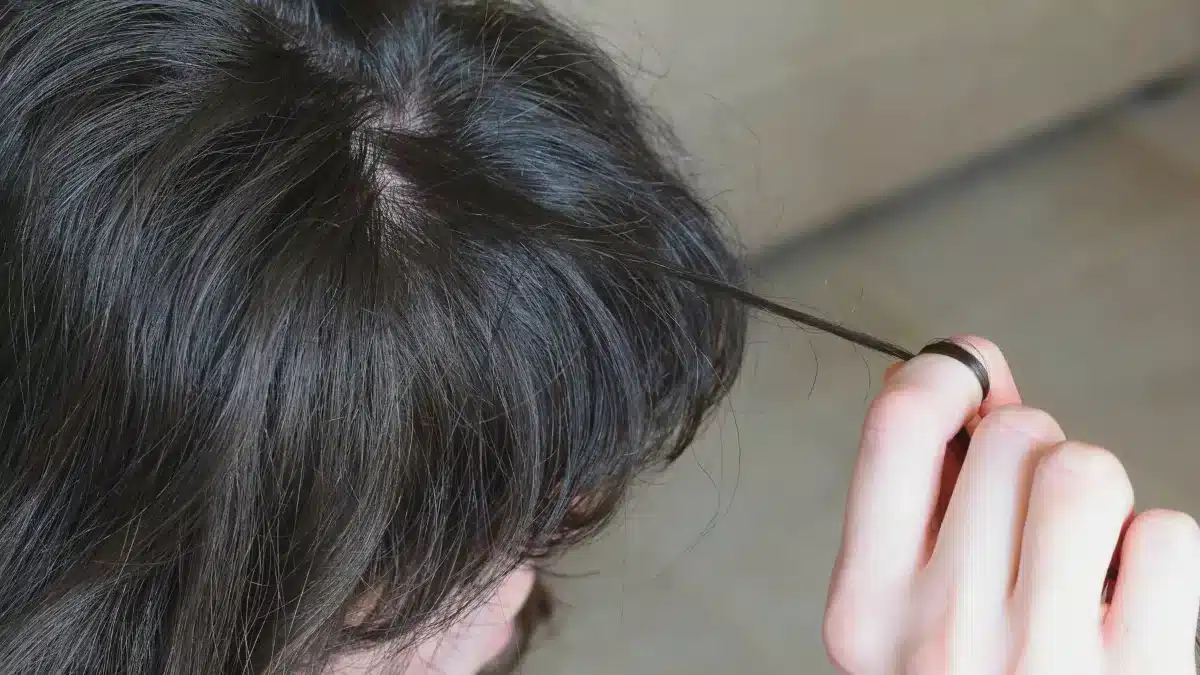
The hair pull test is a common and valuable diagnostic method healthcare professionals use to assess and monitor hair loss disorders in patients.
During this test, the doctor selects around 50 to 60 hairs from a specific area on the patient’s scalp and gently pulls them close to the scalp’s surface.
By doing this, they can observe the number of hairs that come out with minimal force.
The interpretation of the results determines whether there might be an underlying hair loss disorder. |
If more than 10% are pulled out from that particular scalp region, it indicates a potential hair loss disorder or abnormal shedding pattern.
The hair pull test helps differentiate between normal shedding and excessive hair loss.
This could indicate conditions like Alopecia areata, Telogen effluvium, or other hair-related problems.
Uses and effectiveness
The hair pull test is a valuable diagnostic tool in evaluating several hair loss conditions, especially those involving sudden or acute hair shedding.
Here are some specific uses and their effectiveness in different conditions:
Alopecia Areata

Alopecia areata, an autoimmune disorder, leads to patchy hair loss.
The hair pull test is beneficial in monitoring and assessing the advancing edge.
It helps identify areas where the hair follicles are affected, as pulling hairs from these regions may reveal characteristic hair loss patterns.
This information aids in diagnosing the condition and determining the extent of hair loss.
Acute Telogen Effluvium
Telogen Effluvium is characterized by temporary hair loss.
The hair pull test is effective in acute cases of Telogen Effluvium, where the patient experiences sudden and excessive hair shedding.
By pulling hairs close to the scalp, doctors can gauge the number of hairs in the telogen phase, which is higher in this condition, confirming the diagnosis.
Anagen Effluvium
Anagen effluvium is a condition where hair shedding occurs during active growth.
The hair pull test can help identify this condition by revealing the presence of anagen hairs, where the hair shafts are shorter than usual due to premature shedding.
Loose Anagen Syndrome
This hair disorder primarily affects children, characterized by weak hairs that can be easily pulled out.
The hair pull test effectively diagnoses Loose Anagen Syndrome by demonstrating the ease with which hairs can be extracted from the scalp.
In general, a hair pull test aids in diagnosing the underlying cause and guiding appropriate treatment plans.
It helps differentiate between normal hair and excessive shedding, allowing timely intervention and management.
Demerits of hair pull test

The hair pull test, despite being a commonly used method in dermatology and trichology, has several limitations or demerits that need to be considered:
Lack of standardization
The hair pull test is difficult to standardize because different people who do the test might pull with different strengths.
This can cause inconsistent results and make it hard to interpret the findings accurately.
Difficulty in assessing the number of hairs grasped
Approximating the exact number of hairs grasped during the test is often challenging.
This lack of precision can introduce inaccuracies in interpreting the results and lead to false inferences.
Not a standalone diagnostic tool
The hair pull test should not be solely relied upon to make a definitive diagnosis.
It is best used with other diagnostic methods and clinical evaluation for a comprehensive assessment.
Potential discomfort
The hair pull test involves physically pulling hair from the scalp, which may cause discomfort or pain for the patient.
This aspect should be considered, mainly when testing sensitive individuals.
Trichoscopy-assisted hair pull test
Doctors have proposed using a “trichoscopy-assisted hair pull test to enhance the hair pull test.”
Trichoscopy uses a special dermoscopy to examine the scalp and hair closely.
It helps the doctor see things not visible to the naked eye, like the condition of the hair shafts and roots.
When the doctor pulls out some hair, they can immediately use the dermoscopy to look closely at the pulled hair. This allows them to see the roots and shafts in detail.
This new method allows doctors to get more detailed information about hair loss, leading to more accurate diagnoses and better treatment decisions.
It is a non-invasive and valuable tool for evaluating patients with hair loss and a positive hair pull test.
Conclusion
The hair pull test is a valuable and non-invasive tool for assessing and monitoring hair loss disorders.
By observing the number of hairs pulled out with minimal force, healthcare professionals can differentiate between normal shedding and excessive hair loss.
While the hair pull test has proven helpful in diagnosing various conditions, it does have its limitations.
Standardization remains challenging due to variation among practitioners, and the difficulty in assessing the exact number of hairs grasped may lead to false inferences.
Trichoscopy-assisted hair pull test has been proposed as a valuable enhancement to overcome some of these limitations.
Overall, the hair pull test offers valuable insights into hair and scalp health.
Frequently Asked Questions
How much hair is normal for a pull test?
In a normal hair pull test, it is considered normal to have up to 10% of the pulled hairs come out. This means pulling around 50 to 60 hairs from a specific area on your scalp is within the normal range.
What causes a positive hair pull test?
A positive hair pull test occurs when more than 10% of the hairs pulled during the test come out. This can indicate an abnormal shedding pattern or excessive hair loss, possibly caused by various underlying factors.
When should I do my hair pull test?
It is best to consult a doctor to determine if a hair pull test is necessary and when it should be conducted. Consider the hair pull test if you notice a significant increase in hair loss, patchy hair loss, or hair falling out.
What is a negative hair pull test?
A negative hair pull test occurs when fewer than 10% of the pulled hairs come out during the test. In this case, the test does not reveal an abnormal shedding pattern or excessive hair loss. However, a negative hair pull test does not mean certain hair and scalp conditions do not exist.
WowRx uses only high-quality sources while writing our articles. Please read our content information policy to know more about how we keep our content reliable and trustworthy.