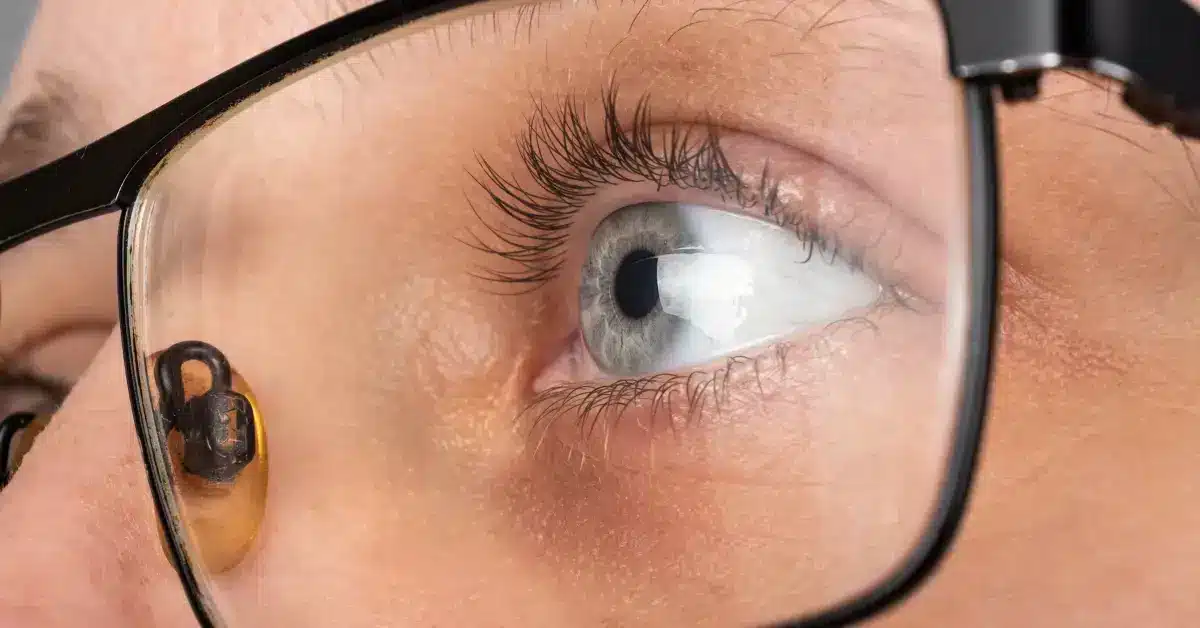
Understanding Corneal Ulcer Stages: A Complete Guide
A corneal ulcer (Bacterial Keratitis) is an open wound on the cornea.
It usually results from an eye infection but can also be caused by other disorders.
According to the Cleveland Clinic, between 30,000 and 75,000 corneal ulcers occur annually in the United States of America.
Corneal ulcers start once the epithelial, the outermost layer of the cornea, is damaged in any way.
This invites bacteria to invade the eye, which might lead to corneal ulcers.
Its progression happens in four stages.
Learn in detail about these corneal ulcer stages further in this article.
Progressive Infiltration

In this stage of Corneal ulcer, the ulcer begins to deepen, causing damage to the corneal tissue.
During this stage, lymphocytes start to move into the epithelium of the tissue.
The following signs of progressive infiltration may appear
- Severe eye pain
- Sensitivity to light
- Redness
- Vision changes
- Gritty feeling in the eye
As the ulcer develops, the affected area may become cloudy.
A yellowish-white discharge may also appear in the eye.
The most significant risk factor at this stage is the potential for the ulcer to perforate or break through the corneal tissue.
Later, it might result in necrosis, depending on how well the body’s defenses work and how dangerous the bacteria are.
The progressive infiltration stage can lead to permanent vision loss if left untreated.
Anyone experiencing symptoms of a corneal ulcer (Bacterial Keratitis) should seek medical attention promptly to ensure proper healing.
Active Ulceration
The active ulceration stage is a critical phase in the development of a corneal ulcer.
During the active ulceration stage, the ulcer continues to progress and deepen, causing increasing damage to the cornea.
The symptoms of an active ulceration stage may be similar to those of the progressive infiltration stage but are typically more serious.
In this stage, there is visible necrosis and sloughing of
- Epithelium
- Bowman’s membrane
- Stroma
Eschar looks like dry, thick, leathery, tan, brown, or black tissue.
Slough is usually yellow, tan, green, or brown in color, and it can look wet, loose, and stringy.
In active ulceration, there is swelling on the walls of the ulcer as the fluid and white blood cells get inside.
The patient might also experience vascular congestion due to the hyperemia of the arteries and the buildup of purulent exudates in the cornea.
It can also cause iritis when the eye takes in toxins, and the iris and ciliary body get clogged up.
Hypopyon is formed when fluid from the iris and ciliary body moves into the anterior chamber.
It is a layering of white blood cells in the anterior chamber.
One of the most significant risks of the active ulceration stage is the potential for the ulcer to perforate the cornea.
If the ulcer progresses in depth, it can lead to the formation of Descemetocele and corneal perforation.
But, lateral progression might lead to Diffuse Superficial Ulceration.
Regression
This stage is triggered by the host’s defense mechanism and the treatment received by them.
During the regression stage, the corneal ulcer begins to heal, and the symptoms associated with the condition begin to improve.
One can notice a line of demarcation developing along the edge of the ulcer where there are more leucocytes than normal.
These leucocytes help to neutralize and phagocyte the necrotic debris and bacteria.
The ulcer might enlarge in the initial stage of digestion of the necrotic debris.
This ulcer enlargement is followed by superficial corneal neovascularization (NV).
NV leads to an increase in the immune response of the host body.
However, it is essential to note that the Corneal Ulcer healing process may take several weeks, and it might take some time for the eye to recover fully.
Cicatrization
The cicatrization stage is the last of the corneal ulcer stages, in which the cornea heals and forms a scar.
This stage occurs after the ulcer has been successfully treated and has gone through the regression stage.
During the cicatrization stage, the cornea continues to heal, and a scar begins to form.
The scar tissue replaces the damaged tissue, and the cornea becomes stronger and more resilient.
However, scar formation might cause vision changes, such as blurriness or distortion.
The amount of scarring during this stage can vary depending on the ulcer’s severity and the treatment’s success.
Regular follow-up appointments with an eye doctor are necessary to monitor the progress of the healing process and ensure that there are no further complications.
Takeaway

Corneal ulcer or Bacterial Keratitis is an open sore on the cornea caused by an eye infection.
It develops through four stages and lasts for about two to three weeks.
The final course of corneal ulcer depends upon the following:
- The aggressiveness of the offending bacteria
- Defense mechanisms of the host
- Treatment received by the host
It is, therefore, important to immediately see a doctor if you suspect that you may have a corneal ulcer.
Early treatment can help prevent the ulcer from progressing and reduce the risk of complications.
Frequently Asked Questions
Does wearing contact lenses increase the risk of a corneal ulcer?
Wearing contact lenses for long periods blocks oxygen from reaching the eyes. Also, the bacteria transferred to the lens while wearing them or from a non-sterile cleaning solution might get trapped in your lens. These factors might cause infections that lead to corneal ulcers.
How long do corneal ulcers last?
Most corneal ulcers heal in about two or three weeks. Your doctor might prescribe you medications depending on the underlying cause of your ulcer. It could be topical, oral, or injections.
Why is my corneal ulcer not healing?
Non-healing corneal ulcers (Indolent Ulcers) are those which fail to heal in the appropriate amount of time. They happen due to an abnormality of the corneal epithelium. This abnormality prevents the epithelium from sticking to the eye’s surface after an injury.
Do corneal ulcers always leave scars?
The corneal ulcer might develop scarring without proper treatment. This scarring might impair your vision or lead to Cataracts or Glaucoma. Therefore, seeking medical attention promptly whenever you have an eye injury is advisable.
WowRx uses only high-quality sources while writing our articles. Please read our content information policy to know more about how we keep our content reliable and trustworthy.